Posted
Categories: Working Together for Better Health Care
The BC Centre for Palliative Care (BCCPC) defines advance care planning as a process of thinking about and sharing your values, beliefs and wishes for future health and personal care with the people you trust. It helps individuals get the care that is right for them, even if they are unable to speak for themselves.1
Advance care planning can ease the burden of making decisions around care options during times of serious illness or injury. As dementia affects decision-making capacity in later stages of illness, there is a window of opportunity for individuals living with dementia to engage in advance care planning conversations and share with family, friends, and health-care providers what matters most to them for their future care. Despite widespread acknowledgement of the importance of advance care planning for people living with dementia, these crucial conversations don’t happen as often as they should.
The Project
To address this challenge, the BCCPC initiated a two-year project in collaboration with key organizations, experts and researchers to encourage people at risk for dementia, or in the early stages of the disease, to engage in advance care planning conversations with their family/friends and caregivers. The project team built on the success of BCCPC’s evidence-based advance care planning model and tapped into the reach of community-based organizations to promote awareness.
“With the help of an advisory committee, expert task group and PVN patient partners, we developed a set of tools, resources and training materials to support community organizations to deliver advance care planning programs tailored for the specific needs of people living with early stages of dementia and family/friend caregivers,” explained Kathy Sheng, the project’s manager.
The project team adapted two existing, community-led advance care planning programs for people living with early stages of dementia and their family/friends caregivers. “My Wishes, My Care…” is a guided group conversation event to help participants explore their values, beliefs and wishes for future health care and personal care. The second program is a two-part information session to teach participants about the steps of advance care planning, including resources to help them get started.
Patient Partner Involvement
Kathy and the team knew that the project’s success hinged on including people who understood the realities of living with or supporting someone with dementia. “Involving people with lived experience throughout the process helped to ensure that the programs and resources designed for them would reflect their values, beliefs, perspectives and needs,” she explained. To do so, they enlisted the help of nine PVN patient partners from across BC.
Patient partner Doreen F was interested in the project because of her family’s own experience with dementia. “We were completely unprepared when my mother-in-law was diagnosed, and many feelings such as denial, guilt, sadness and loss made it all the more difficult to put an effective plan in place. We would have benefited from advance care planning, and so I was pleased to see information sessions being offered. I wanted to be part of helping others who may one day face this challenge,” she shared.
From April to August 2020, patient partners contributed to the project in several ways, including sharing personal insights and perspectives on the barriers and facilitators they encountered when engaging in advance care planning conversations. That invaluable information helped to inform the program’s curriculum content, instructional design, learning environment and communication strategies. Some of the insights shared by patient partners which were later incorporated into the design of the programs include:
- Emphasizing advance care planning conversations rather than completing forms
- Using storytelling to share information
- Providing easy-to-use ways to start advance care planning conversations
- Providing a concrete, step-by-step approach to advance care planning
“Patient partners also provided feedback on the design, usability and content of our public-facing materials,” said Kathy. “Their feedback helped to address the readability of marketing posters and public-facing handouts, interpretation of advance care planning-related icons designed for visual learners, usability of online evaluation surveys and relatability of resource content.”
The Pilot & Early Outcomes
“To launch and evaluate the tailored advance care planning programs in the community, we used a stepped approach: first a focused pilot, then a wider implementation. At both stages, we partnered with community-based organizations to deliver the two programs in their communities.
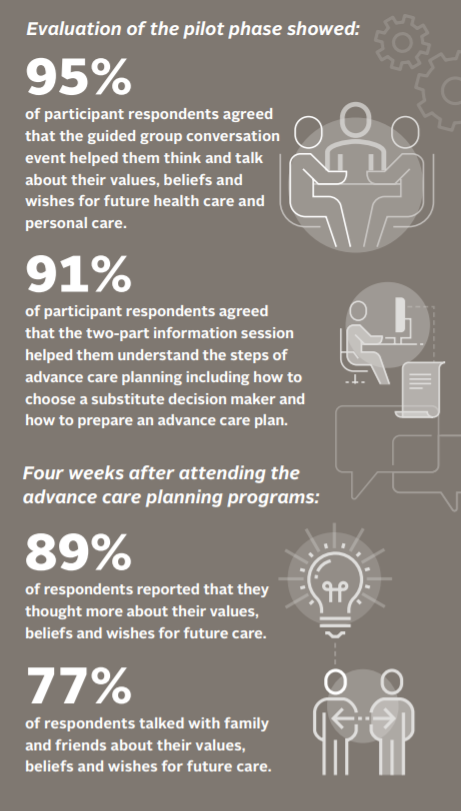
BCCPC provided each organization with training, a comprehensive toolkit of resources, and ongoing coaching to support them with program delivery and sustainability,” shared Kathy. Following a successful pilot phase with four community-based organizations in the spring of 2021, the programs were refined and rolled out in partnership with 10 organizations in BC. Plans are underway for a knowledge translation phase in late 2021 to share the finalized advance care planning programs and lessons learned throughout BC and other jurisdictions.
To date, over 40 staff and volunteers from community-based organizations have been trained as advance care planning program facilitators. The input from the community organizations, facilitators, and public participants was an important element to the success of the programs.
Engagement Tips
Doreen commented on the excellent communication and clear expectations for patient partner participation that contributed to the engagement’s success. “I’ve been involved in quite a number of opportunities as a PVN volunteer and I found this engagement to be very positive,” she said. “I appreciated all the information provided and that it was made easy for someone with limited computer software to access,” she added, noting the importance of taking technology into account when making engagement opportunities accessible for patient partners.
The project tried to minimize technological barriers associated with online platforms such as Zoom. “Instead of online focus groups, patient partners were engaged in a one-on-one manner via phone or email, and were sent information, questions, and materials at least two weeks in advance so they could prepare their responses,” Kathy added. She also reflected that conducting the engagement activities remotely also helped to connect with patient partners who would otherwise not have been able to participate in person.
Advice for others? Kathy says, “To the greatest extent possible and through multiple levels of public engagement, involve patient partners and those with lived experience in decisions and initiatives that impact them.” On that note – there will be more engagement opportunities to come for the project. If you are a person living with dementia or a family/friend caregiver of a person living with dementia, and you wish to get involved, please email kathysheng@bc-cpc.ca. For more information about the project, visit bc-cpc.ca.
This story was featured in our 2020/21 Annual Report. Read more like it here.
1 BC Centre for Palliative Care. Advance care planning [Internet]. 2021 [cited June 15 2021]. Available from: https://bc-cpc.ca/allresources/individuals/acp/


