Posted • Last updated
Categories: Improving Health Care, Patient Voice Mail, Working Together for Better Health Care
In the fall of 2020, a Palliative Care – Partners, Services and Transitions Shared Care project was created in the North Okanagan, specifically in Vernon and surrounding areas. A project team and an advisory group rolled up their sleeves for a series of meetings, interviews and surveys through August 2021.
Palliative care is a sensitive subject but an essential component of health care.
Project Synopsis
The goal of this work was to develop a new model of palliative care and define future processes that better support persons, families and caregivers in their journeys. The work needed to include defining patient, family and caregiver needs, understanding the current state of palliative care in the region, identifying gaps and creating a plan to improve processes.
Defining Palliative Care
Broad ideas posed by the person, family and caregiver partners helped form the direction of the project, starting with the need to define “palliative care,” a term which is often incorrectly associated only with end-of-life care. (This project uses the term “person, family and caregiver partners” to describe the project’s team as it best describes the variety of perspectives brought to the table.)
Palliative care is the special care of a person whose life-limiting serious illness or disease cannot be cured. It may encompass the span of time between diagnosis of a palliative condition through end of life.
The Advisory Group
The advisory group included people with palliative conditions, caregivers and family partners who shared their experiences, ideas and suggestions for palliative care improvement through an interview and/or by completing a survey. Their input and feedback also helped to identify gaps in care. For example, when the group compared how service providers (nurses, doctors, program administrators) and person, family and caregiver partners rated the current state of palliative care, it learned that person, family and caregiver partners thought their needs were always, often or sometimes met 60% of the time. On the other hand, providers felt that this happens 80% of the time.
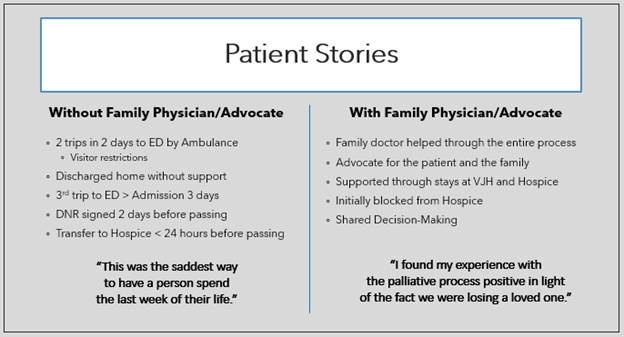
The group also learned that person, family and caregiver partners’ palliative care experiences, especially near end of life, were very polarized – either good or very challenging – and that both types of experiences were truly memorable.
The Project Team
The project team came together regularly to understand what was currently happening, establish an ideal future for palliative care in the Vernon area and identify opportunities for improvement. That led to the creation of an action plan to take incremental steps to achieve the future vision. There were a broad number of service providers and stakeholder organizations involved.
“Having partners who are currently experiencing a palliative condition provided rare insight into the palliative care experience.” – Diane Edlund, Project Co-Lead
Patient Influence
There are many examples of how patients influenced the project, including how the impact of their stories about multiple ambulance trips to the hospital prompted the advisory group to invite BC Emergency Health Services to participate in the project. The participants also ensured that the action plan and future vision always respected diversity of culture, race and gender as well as hardly reached or unconnected populations, including people living in rural or remote areas and people with less access to technology.
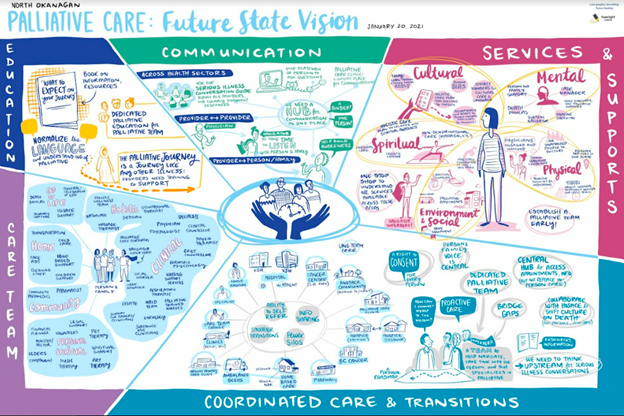
Future State Vision
The person, family, and caregiver partners were particularly helpful in setting the direction of the future state vision for palliative care in the North Okanagan. While service providers on this project continuously referred to the “palliative care team,” they quickly learned that not all persons and families experience a cohesive, multi-disciplinary team. It was surprising when a family member posed the question, “There’s a team?” This input created the motivation to explore what makes an ideal palliative care team as part of the future vision.
Identifying Partners
While the project leads thought that many family members and caregivers would want to come forward to share their experiences, it’s important to acknowledge that this was quite difficult for the few that did. Everyone associated with the project felt the person, family and caregiver partners were brave for speaking up and sharing their stories.
Sensitive Subject Matter
Diane Edlund, the Project Co-Lead, shared that palliative care can evoke feelings for everyone, especially if their experience is current or recent. She wanted to make sure that everyone took care of themselves during this work. It was important for the team to be sensitive to the subject matter with open and honest communication channels. Additionally, a process was developed for partners to opt out of specific discussions they felt were too difficult or to opt out of the project entirely.
Project Outcomes
The project team was pleased that the outcome was achieved. An action plan, together with a new model of care, was created for palliative care which encompasses services and supports for persons, families and caregivers, service provider roles and relationships, training needs and actions to smooth transitions between care settings and levels of care.
Evaluations
Participants shared that the project was extremely well-run and organized, and that its leads were terrific about communicating with everyone and keeping everyone’s voice in the project.
Supporting Future Projects
Diane is happy to connect with other teams working on palliative care projects which have similar deliverables, and to share what she learned from working with and engaging people with palliative conditions as well as families and caregivers. Diane can be reached at d.edlund@telus.net.
Patient Stories & Next Steps
Hearing peoples’ stories ensured that the focus of the project was person-, family- and caregiver-centred. One of the great achievements of this action plan was suggested by two patient partners who met independently to support each other. A repository of patient stories will be gathered for service provider education and for centring or grounding palliative care meetings in purpose. The best part is that this follow-on project is being led by a patient partner!
Sharing Your Story
If you have a palliative care story to share or would like to assist in gathering person, family and caregiver stories, please contact Colleen Foran at colleen.foran@gmail.com.
Author: Carol Stathers, Engagement Lead, BC Patient Safety & Quality Council & Diane Edlund, Project Co-Lead