Posted
Categories: Building Skills, My Experience, Patient Voice Mail
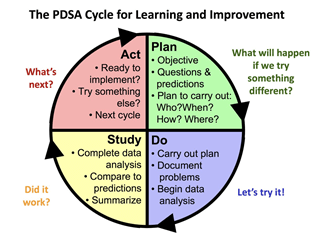
Do plan-do-study-act (PDSA) cycles, run charts and the Model for Improvement leave you scratching your head? These terms have become common language for those attending the Institute for Healthcare Improvement (IHI) Open School Basic Certificate in Quality and Safety.
Continued learning is a great perk of being a patient partner with the Patient Voices Network, and over the years we have provided opportunities to attend education opportunities such as San’yas Anti-Racism Indigenous Cultural Safety Training Program, the Beryl Institute’s Patient Experience Conference and the BC Patient Safety & Quality Council’s Quality Forum.
We started offering the IHI Open School Basic Certificate to patient partners in May 2019 and since that time, have sponsored 91 patient partner participants over a series of five cohorts.
For those looking to expand their knowledge and skills about quality improvement practices in health care, this online learning opportunity provides essential training and tools on the topics of improvement methods, measuring change, patient safety and more.
Learning From Those With Lived Experience
Following completion, we ask participants to share their key takeaways from the course. Leanne Varney shared that she learned about the models of health care improvement and expanded her perspective of what innovative and integrative care can look like. It was particularly interesting to learn about health care improvements from those who have lived experience and knowledge of shortcomings that exist in the current system. In the module focused on responding to adverse events, she thought it was neat to see how even in the direst of situations, when built upon a framework of honesty and patient safety, the response to a variety of events is similar.
Planning Change in Incremental Steps
Thelma Boileau acknowledged that health care is a complex system, and that making changes is difficult and requires broad input from all levels. Changes need to be made and planned in small incremental steps. Then, the results need to be studied before further action.
We also asked patient partner participants to share their aha moments when reflecting on the course.
Reaching an Aha Moment
Darla Biagioni shared that one of her aha moments was thinking about patient care from the view of patients – similar to the “What Matters to You?” initiative. She recognized that not every person, or situation, can fit into a tidy little box. Health care staff don’t know what patients are dealing with before they arrive.
Uriah commented that she learned that every failure is an opportunity for learning and improvement. This helps prevent mistakes from happening again to another patient and draws attention to meeting standards.
Bringing New Skills into Future Activities
We were also curious to learn more about how patient partner participants would use the skills they learned and how this learning opportunity may support their future patient engagement activities.
Leanne Varney said that she’ll bring more insight into conversations to increase the likelihood that different aspects of care are addressed when working to improve health systems.
As a patient partner, Mariana da Silva Jardim feels that knowing the important steps before a change is adopted and an aim is reached will allow her to feel more comfortable when engaging with quality improvement opportunities. It’ll also allow her to better formulate her ideas and opinions when discussing health care improvements.
Moving forward, Thelma Boileau has a better understanding of the complexities of health care systems and an appreciation of how difficult it can be to make changes to procedures and programs. Input from all stakeholders is important, including patients, families and caregivers. She also has a better understanding of quality improvement and PDSA cycles, which will help to understand the process of change and who should be involved in the planning. To receive the certificate, participants must complete the 13 Open School courses on topics such as Improvement Capability, Patient Safety, Triple Aim for Populations, Person- and Family-Centred Care and Leadership.
Improvement Capability Topics:
- Introduction to health care improvement
- How to improve with the Model for Improvement
- Testing and measuring changes with PDSA cycles
- Interpreting data: run charts, control charts and other measurement tools
- Leading quality improvement
Patient Safety Topics:
- Introduction to patient safety
- From error to harm
- Human factors and safety
- Teamwork and communication in a culture of safety
- Responding to adverse events
For more information and an overview of the course, check out IHI’s website!
Stay tuned for more opportunities to participate in educational sessions. Once we have a new cohort starting for IHI’s Open School, we’ll provide the details in our Engagement Opportunities newsletter.
Author: Carol Stathers, Engagement Lead, BC Patient Safety & Quality Council