Posted • Last updated
Categories: Patient Voice Mail, Working Together for Better Health Care
What makes patient engagement successful? How do we know if it’s ‘good’ or ‘working well’? Despite the growing momentum and practice of patient engagement in quality improvement, system redesign, and other health system projects, there remains no widely agreed upon way to determine how well, or if these efforts are working. It’s something Dr. Clayon Hamilton would like to see change.

Clayon is the Regional Practice Lead in Research & Knowledge Translation for Long-Term Care in Fraser Health. For a number of years he has been working to advance the practice of measurement and evaluation in patient engagement. As a post-doctoral fellow at UBC in 2015-2020, Clayon and his collaborators produced the (PEIRS) framework¹ and scale², which are now well utilized tools in health research for evaluating the quality of patient-researcher partnerships.
In 2018, Clayon’s efforts expanded from the health research sector to health systems more broadly, to explore how, and how well, patients and family caregivers were being engaged in health system decision making. He was awarded a CIHR-MSFHR Health Systems Impact Fellowship at the BC Ministry of Health to help evaluate the engagement component in the Patients as Partners (PasP) initiative – a collection of programs in several organizations working to promote person- and family-centered care in BC.
Defining success in patient engagement in health systems decision-making
“We started by asking how we would define success of patient and family caregiver engagement in health system decision making. We needed a framework to do that, and nothing existed at the time. There wasn’t a strong evidence base to draw on,” explained Clayon. “We quickly realized this would be more work than anticipated!”
The team decided to start with a scoping review of the literature to review and identify key elements that could define success in patient engagement. The study protocol³ was published in 2019 and the completed study was published in 2021.⁴
Patients Included
In the second year of the project, two PVN patient partners were welcomed to the team: Vikram Bubber and Allison Kooijman.

Vikram was keen to contribute to a project that would help to articulate successful patient engagement and describe its outcomes, to help build the business case for patient engagement. “Decision makers need to be able to see if what is being done – is working, or not working. We might automatically think that patient engagement is important – but they are always looking at costs, and whether there is any benefit.”
Allison enjoyed the research aspect of the project. “I think it’s important for patients to be involved in the development of knowledge in this area – which is what we did in this work with Clayon. I was keen on the mechanism by which we could think about and measure successful patient engagement,” she shared.
Clayon explained that Allison and Vikram joined the project after the literature review was underway – “at a point in the project where they could inform the data analysis and help to interpret the data. We really needed to ensure that we were capturing patient partner and family caregiver perspectives – because this is a framework geared towards defining the success of their engagement in health system decision making,” said Clayon.
Allison agreed. “A lot of this work was technical, but there was a huge interpretive piece, which is where we were able to contribute – reframing information and bringing a patient lens to it all,” she added.
In addition to data analysis and contributing to the development of the framework, Allison and Vikram participated in writing an article to be submitted for publication, and Allison co-presented about the project at Quality Forum 2021.
The Framework: 18 Key Themes for Successful Engagement
The result of their work was the development of a preliminary framework “Engagement of patients and family caregivers (PFCs) in healthcare system decision-making”.⁴ The 18 key themes fall under three broad categories: structure, process and outcomes and help to describe the components of what ‘successful engagement’ should include. The framework lays the groundwork for future evaluation work: developing logic models and mechanisms to evaluate patient and family caregiver engagement initiatives.
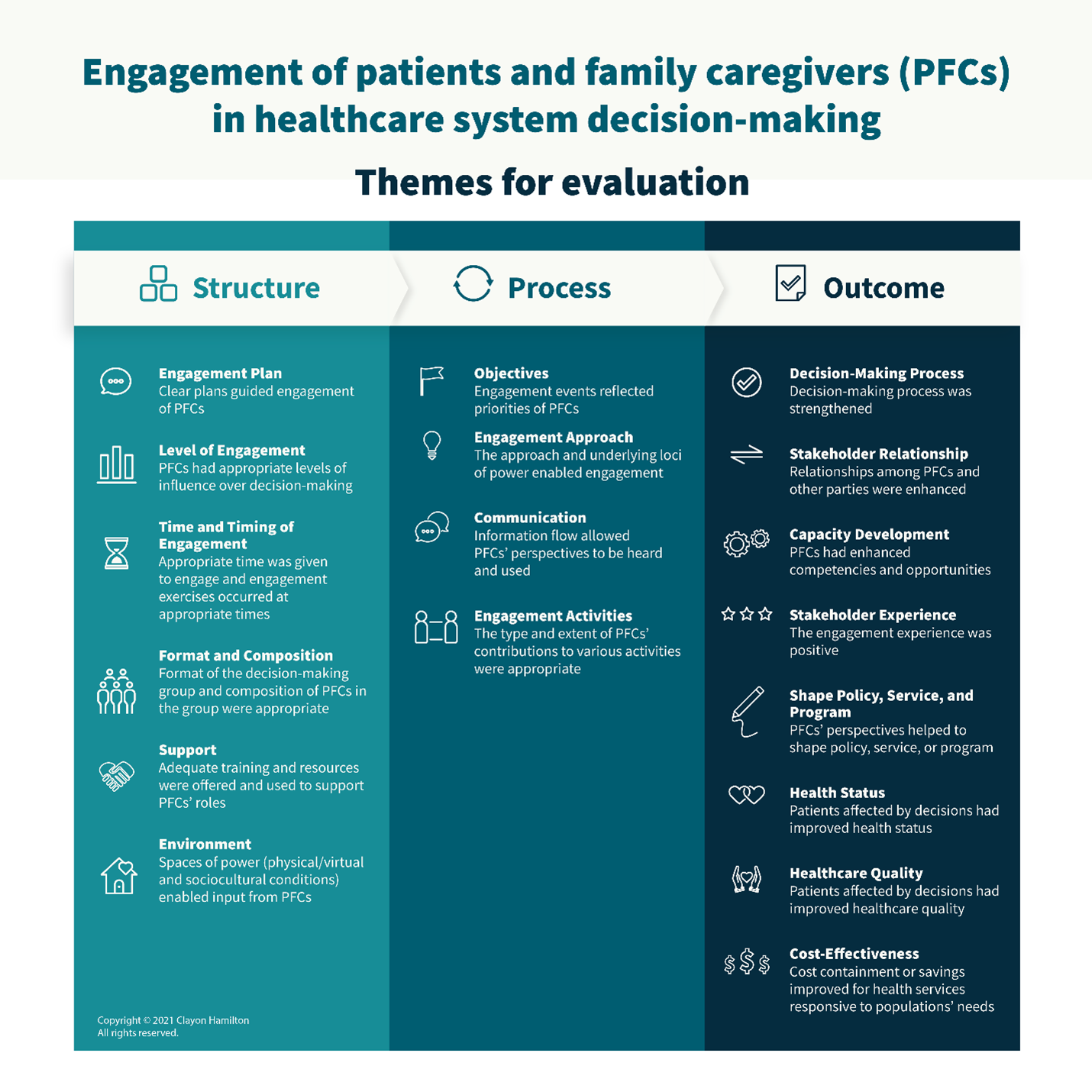
“It was actually Allison who brought forward Stakeholder Experience as an important engagement outcome to include in the framework. We hadn’t considered that, and then we realized we should ensure that all of the quadruple aim should be included as outcomes,” said Clayon.
“We don’t know what it would have looked like without the patient partners, but I feel like with them involved, we are shaping something that makes sense, from various perspectives, most importantly from their perspectives – defining the themes of what quality engagement looks like.”
A Solid Working Relationship
Both Vikram & Allison commented on how approachable and inclusive Clayon was in their work together.
“We could talk freely. If I didn’t understand something that had been sent to me – I could just contact him to clarify,” recalled Vikram. “He was willing to continually engage with us and took time to make sure we understood some of the bigger overall concepts, which he understands so well from his background in research”.
Allison appreciated the many opportunities to provide input. “I really felt like he cared about what I had to say,” reflected Allison. “It was a very well done, robust consultation. It didn’t feel tokenistic at all,” she shared.
Next Steps
What’s next? The team hopes to build on the 18 themes and create a provincial framework for patient and family engagement in health system decision-making. Clayon, along with Tammy Hoefer (BCPSQC) and Beth Snow (CHEOS) have recently applied for a research grant, which they hope will enable them to bring together engagement specialists from across the province to expand on the themes, develop a more fulsome evaluation framework with an implementation plan to roll out across BC. Eventually they’d like to do more research on the topic too.
This story was featured in our 2021/22 Annual Report.
[1] Hamilton C, Hoens A, Backman C, et al. (2018) An empirically based conceptual framework for fostering meaningful patient engagement in research. Health Expect. 21:396-406.
[2] Hamilton C, Hoens A, McKinnon A, et al. (2021) Validation of the Patient Engagement In Research Scale (PEIRS) for measuring meaningful patient and family caregiver engagement. Health Expect. 00: 1– 17.
[3] Hamilton C, Snow ME, Clark N, et al. (2019) Quality of patient, family, caregiver, and public engagement in decision-making in healthcare systems: a scoping review protocol. BMJ Open, 9(11).
[4] Hamilton C, Dehnadi M, Snow ME, Clark N, Lui M, McLean J, Kooijman A, Bubber V, Hoefer T, Patients as Partners Team, Li LC. (2021) Themes for evaluating the quality of initiatives to engage patients and family caregivers in decision-making in healthcare systems: a scoping review. BMJ Open.
Author: Kira Tozer, Leader, Strategic Initiatives, Patient & Public Engagement

