Posted • Last updated
Categories: My Experience
PVN Patient Partner Chad Dickie was recently sponsored by PVN to attend a great learning opportunity: a workshop on Design Thinking facilitated by the BC Patient Safety & Quality Council. Chad has been a volunteer since 2017 and has been a part of several committees and Boards, and involved with multiple patient engagement opportunities. He recently won the 2019 Quality Award for Leadership in Advancing the Patient Voice. He has written a blog post about his experience at the workshop and how he`ll apply his new knowledge to his future engagements. Take it away, Chad!
When I saw a recent engagement opportunity for the Design Thinking workshop in Victoria, I immediately applied for a PVN-sponsored seat and was fortunate to be selected to attend. So, on a rainy day in November 2018, I joined 22 healthcare professionals and our facilitators, Anthony Gagne, Kathryn Proudfoot, Colleen Kennedy and Andrew Siu, for a full-day introduction to design thinking.
Identifying a Problem to Be Solved

Before the start of the workshop, I had homework: I was asked to think of a “wicked problem” or a challenge that can be turned into an opportunity for change. I decided I wanted to use this workshop to think about how to embed patient and peer navigation in primary care to improve the patient experience.
The presentation revolved around a few main topics, focusing mainly on different ways to cultivate empathy for better communication and improving services, as well as the ways design thinking matches human needs with available resources. We discussed using interview techniques to identify improvement needs and how to turn ideas into action.
The Importance of Empathy in Health Care
We dug deep into empathy as it’s essential to effective interpersonal communication and a human-centred approach in health care and beyond. Being empathetic can help identify users and their issues and needs, provide guidance for identifying behavioural patterns, and generate inspiration on appropriate and conscientious response to others, whether a patient, client, co-worker or supervisor.
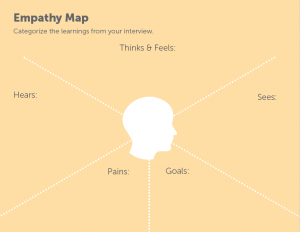 The workshop introduced me to some new concepts for innovative thinking such as empathy mapping and techniques called SCAMPER (substitute, combine, adapt, modify, put to another use, eliminate, reverse) and Building to Think. I learned that some of the biggest motivators for change come from the dialogue to uncover needs, being aware of power dynamics, leap-frogging off other ideas and leading alongside patients and families.
The workshop introduced me to some new concepts for innovative thinking such as empathy mapping and techniques called SCAMPER (substitute, combine, adapt, modify, put to another use, eliminate, reverse) and Building to Think. I learned that some of the biggest motivators for change come from the dialogue to uncover needs, being aware of power dynamics, leap-frogging off other ideas and leading alongside patients and families.
What I’ll Bring Back to my Volunteering
The workshop was fast-paced but it was an enjoyable day of learning and engaging with others. My biggest takeaway from Design Thinking is that it is easier to work a ridiculously big idea down to a manageable solution than it is to build up a mediocre idea. As a PVN patient partner, this workshop will help me challenge myself to improve my constructive contributions in BC’s health care system as a patient, caregiver, researcher and life-long learner. Thank you, PVN, for selecting me to attend the Design Thinking: A Human-Centred Approach to Health care Improvement workshop.
Thanks for sharing your experiences, Chad! You can follow Chad on Twitter at @chaD4quality.


